The Silent Fortress: Why Men Would Rather Face Anything Else Than a Doctor’s Exam

There is a specific kind of silence that exists in the locker rooms, hunting lodges, and bars where men congregate. It’s not an empty silence; it’s a heavy one. We talk about the torque of a new engine, the failure of a secondary defense, the rising cost of ammunition, or the shifting geopolitical landscape.
We might even touch on the "safe" health topics—a torn ACL, a persistent cough, or the grueling recovery from a back injury. These are badges of honor, proof of a life lived with intensity.
But there is a perimeter we rarely cross. When the conversation drifts toward the foundational aspects of our biology—specifically, the health of our reproductive organs—the shutters come down. The bravado thins. We retreat into a stoicism that, while culturally ingrained, is increasingly at odds with our long-term survival and quality of life.
The question isn't just why we stay quiet; it’s what that silence is costing us. To understand why men hesitate to discuss genital health, we have to look past the surface-level embarrassment and examine the intersection of biology, heritage, and the modern male identity.
The Weight of the "Engine Room"
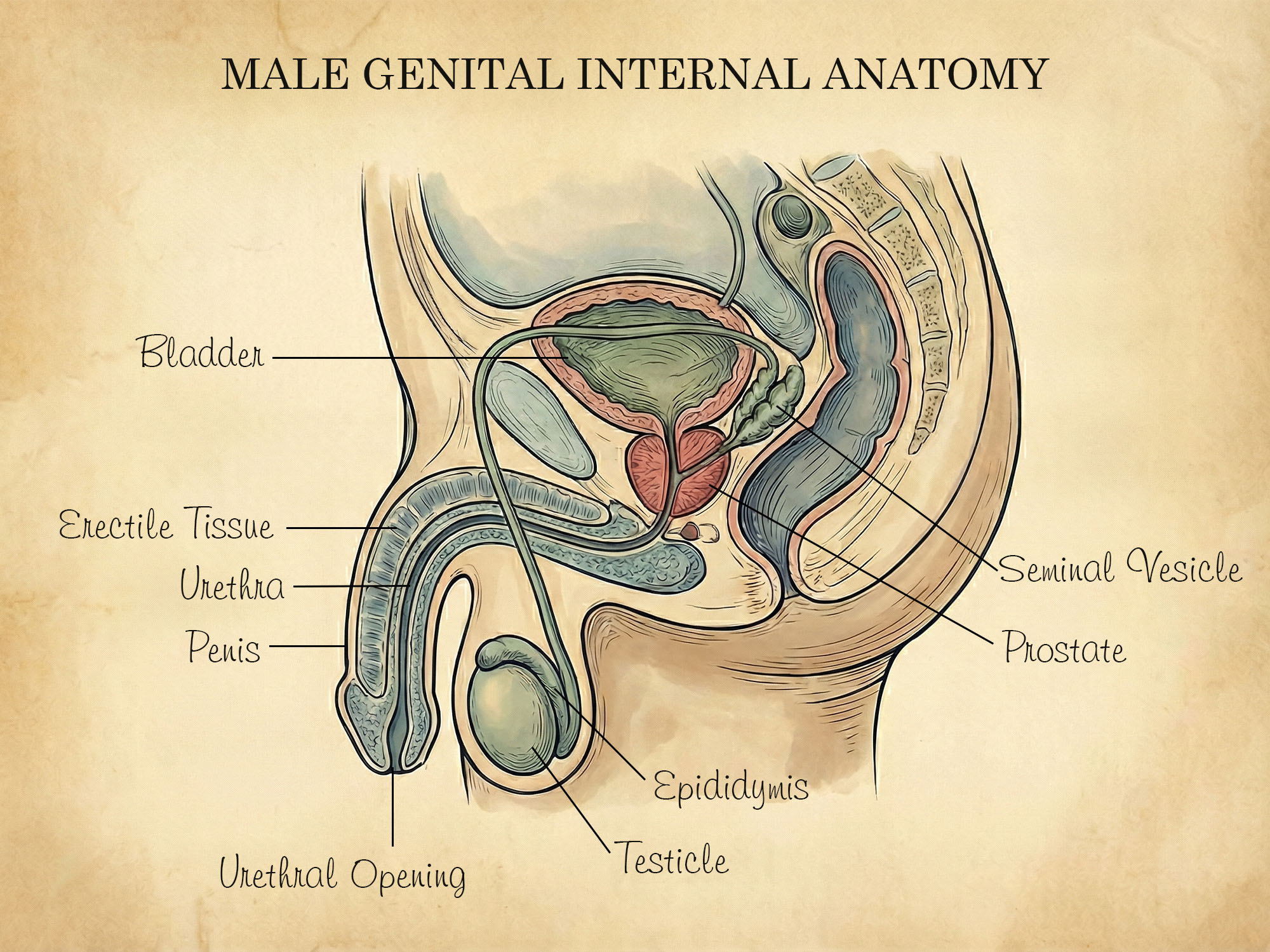
For a man, his genitals are rarely viewed as just another organ system, like the lungs or the liver. They are the "engine room" of his existence. From a young age, we are taught—often implicitly—that our worth is tied to performance, protection, and provision. The male anatomy is the physical manifestation of that potential. It is the source of our testosterone, the driver of our ambition, and the mechanism of our legacy.
When something goes wrong in that department, it doesn't feel like a medical glitch. It feels like a systemic failure. To admit to a bump, an ache, or a decline in function is, in the primitive corners of the male brain, an admission that the core of our "machinery" is compromised.
This is the first wall of hesitation: The Identity Barrier. If the engine is smoking, the whole truck is down. Rather than face the reality of a repair, many men prefer to keep the hood closed and hope the noise goes away on its own. It is a gamble we take to preserve our sense of self, even when the odds are stacked against us.
Common Concerns vs. Rationalizations
| Physical Symptom | Common Hesitation | The Practical Action |
|---|---|---|
| Painless Lump | "It doesn't hurt, so it's fine." | Urgent Urological Review |
| Performance Decline | "I'm just stressed or tired." | Hormonal & Vascular Screening |
| Urinary Changes | "Part of getting older." | Prostate Health Baseline |
The Legacy of the "Strong, Silent" Type
Cultural Insight
"In ancient Sparta, health was a civic duty. To be unfit or unwell was seen as a failure of your obligation to your brothers-in-arms. Today, we often confuse 'toughing it out' with 'negligence.' Real strength has always been about readiness."We live in an era that frequently critiques traditional masculinity, yet the biological and historical roots of the "strong, silent" archetype remain potent. For generations, men were the scouts, the soldiers, and the laborers. In those roles, showing vulnerability was not just discouraged; it was dangerous. A man who complained about his health was a liability to the group.
While we are no longer fending off wolves or clearing forests by hand, that ancestral hardwiring persists. We carry a cultural DNA that equates silence with strength. Discussing a sensitive health concern feels like a "leak" in our armor.
Furthermore, the clinical environment itself is often perceived as inherently emasculating. The transition from being a self-sufficient man in the world to a "patient" in a paper gown is a jarring shift in status. In a doctor’s office, you are no longer the one in control. You are being poked, prodded, and questioned. For many men, the discomfort of that power dynamic is enough to keep them from booking the appointment in the first place.
The Gap in Health Literacy

There is also a functional issue at play: many men simply don't have the vocabulary for these conversations because they weren't given it.
Think back to your upbringing. Most boys receive a rudimentary "health class" talk that focuses on the mechanics of reproduction or the avoidance of disease, usually delivered with a side of awkwardness that ensures no one asks a follow-up question. Women, by contrast, are often introduced to the healthcare system much earlier and more consistently. From the onset of puberty through childbearing years, women are encouraged—and often required—to maintain a regular dialogue with specialists.
Men have no such equivalent. Once we outgrow the pediatrician, many of us enter a "medical wasteland" in our twenties and thirties. We only see a doctor when something is broken. Consequently, we never develop the habit of preventative maintenance. By the time a man notices a change—perhaps a dull ache in the scrotum or a change in urinary habits—he lacks the rapport with a physician to bring it up casually. It becomes a "big deal" because we haven't made it a "normal deal."
The Fear of the Worst-Case Scenario
Hesitation is often fueled by a specific brand of anxiety: the fear of what we might find. In the male mind, a small concern can quickly spiral into a catastrophic conclusion.
-
That lump? It’s definitely cancer.
-
That performance issue? My testosterone is gone, and I’m "over the hill" at 40.
-
That skin irritation? It’s a permanent mark of shame.
We tend to think in binaries—functioning or broken, healthy or dying. This "all or nothing" mindset makes the stakes of a medical conversation feel incredibly high. If we don’t talk about it, the "catastrophe" isn't official yet. We can maintain the status quo.
"We treat our bodies like high-performance machines until they falter, then we treat them like secrets. True resilience lies in the maintenance, not the avoidance."
This is particularly true regarding conditions like Testicular Cancer, which primarily affects younger men between the ages of 15 and 35. It is one of the most treatable forms of cancer if caught early, yet the survival rate depends entirely on a man’s willingness to perform self-exams and speak up when something feels off. The hesitation to speak doesn't just prolong discomfort; it can literally be the difference between a minor procedure and a life-altering battle.
The Role of Modern Performance Pressure
In today’s world, the pressure on men has shifted from pure physical labor to a more complex "performance" expectation. We are bombarded with images and messages about "optimization." We are told we need to have the highest T-levels, the lowest body fat, and the most stamina.
In this culture of "optimization," genital health concerns are seen as the ultimate setback. There is a profound social stigma around issues like erectile dysfunction (ED) or Peyronie’s disease. Despite the fact that ED is often a vascular issue—a "canary in the coal mine" for heart health—it is still treated as a punchline or a source of deep personal shame.
When we treat these issues as "failures" rather than "medical conditions," we drive men further into isolation. A man is much more likely to seek out a "quick fix" pill from an unregulated online source than he is to sit down with a urologist and discuss the underlying cause. We would rather self-medicate in the dark than seek professional guidance in the light.
Breaking the Code of Silence
So, how do we move forward? How do we maintain our masculine identity while acknowledging that our bodies require maintenance?
The shift begins with a change in perspective. We need to stop viewing genital health as a separate, "shameful" category of wellness and start seeing it as the foundation of our overall performance. A man who monitors his heart rate, his bench press, and his macros but ignores his reproductive health is not "tough"—he is being a poor steward of his most important asset.
1. Reframe the Conversation
We need to talk about genital health in the same way we talk about any other high-performance system. You wouldn't ignore a "Check Engine" light on a classic car or a crack in the foundation of your home. Taking care of your "engine room" is a matter of discipline and responsibility. It’s an act of leadership—taking charge of your health so you can continue to provide for your family and lead your life.
Quick-Start: The Maintenance Protocol
- Schedule a yearly physical.
- Track changes in energy and libido.
- Speak honestly with your physician.
- Don't self-diagnose via forums.
- Don't buy unregulated 'T-boosters'.
- Don't wait for pain to manifest.
2. Standardize the Check-Up
We should encourage a culture where an annual visit to a urologist is as standard as a dental cleaning. When something is routine, the "weight" of the conversation disappears. We need to normalize the "oil change."
3. Peer Accountability
This is where the "locker room" dynamic can actually be a force for good. We don't need to get graphic or overly emotional, but we can normalize the idea of health maintenance. If a friend mentions he’s been feeling run down or "off," the response shouldn't be a joke; it should be, "Have you had your bloodwork or a physical lately?" Real brotherhood involves looking out for the longevity of the men next to you.
Common Questions on Men's Health
At what age should I start seeing a urologist?
While there is no "set" age, having a baseline check-up in your 20s or 30s is wise. Regular prostate screenings typically begin at 50, or 45 if you are at higher risk.
Is ED always a psychological issue?
No. While stress plays a role, ED is frequently a physical symptom related to blood flow, heart health, or testosterone levels. It should be treated as a medical indicator, not a mental failure.
How often should I perform a self-exam?
Once a month is recommended. The best time is after a warm shower when the muscles are relaxed. Familiarity with your own anatomy is the best way to spot changes early.
The Way Forward: Strength in Awareness
The reality is that women have been ahead of us on this for decades. They have built networks of support, normalized regular screenings, and stripped away much of the mystery surrounding their health. It hasn’t made them "weaker"; it has made them more resilient and longer-lived.
For men, the path to better health doesn't require us to abandon our ruggedness or our privacy. It requires us to apply that same ruggedness to our self-care. It takes a certain kind of courage to walk into a doctor's office and say, "Something isn't right," especially when every instinct tells you to hunker down and ignore it.
We need to realize that the "Silent Fortress" we build around our health doesn't protect us; it traps us. It prevents us from accessing the very tools that can keep us in the game longer.
The next time you feel that hesitation—that urge to stay silent about a concern "below the belt"—remember that true masculinity isn't about being indestructible. It’s about having the wisdom to maintain the machine, the strength to face the facts, and the responsibility to ensure you’re around for the long haul.
Your health is the foundation of your legacy. Don't let silence crumble it.
Key Takeaways for the Modern Man
| Concern | Why We Hesitate | The Reality |
|---|---|---|
| Lumps or Growths | Fear of a life-altering cancer diagnosis or loss of virility. | Most abnormalities are benign; however, early-stage testicular cancer has a 95% cure rate. Silence is the only real danger. |
| Performance Issues | Deep-seated ego bruising; viewing ED as a personal failure. | Often a "canary in the coal mine" for heart health or vascular integrity. Treating the cause protects your life, not just your ego. |
| Persistent Aches | The "tough it out" mentality; assuming pain is a normal part of aging. | Chronic discomfort can signal infections or varicocele, which can impact testosterone production and long-term fertility if left untreated. |
| Hormonal Shifts | Anxiety regarding "getting old" or losing a competitive edge. | Optimizing T-levels through medical guidance improves mental focus, muscle retention, and metabolic health. It is an act of maintenance, not weakness. |
Disclaimer: The articles and information provided by Genital Size are for informational and educational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition.


 日本語
日本語  Deutsch
Deutsch  English
English  Español
Español  Français
Français  Português
Português 


